Analysis of human brain tissue reveals differences in how immune cells behave in the brains of people with Alzheimer’s disease compared to healthy brains, suggesting a potential new therapeutic target.
The discovery was made by research led by the University of Washington, which was published in August Microglia cells In the brains of people with Alzheimer’s disease In a proinflammatory state Often, making them less vulnerable to protection.
Microglia are immune cells that help keep our brains healthy by removing waste and maintaining normal brain function.
In response to infection or to remove dead cells, these elegant, shape-shifting shapes can become less rotating and more mobile to engulf invaders and trash. them too Synapses “prune” during developmentwhich helps form the circuits that help our brains function well.
It is not certain what role they play in Alzheimer’s disease, but in people with this devastating neurodegenerative disease, some microglia respond very strongly. May cause inflammation Which contributes to the death of brain cells.
Unfortunately, clinical trials for Anti-inflammatory drugs for Alzheimer’s disease have not shown significant effects.
To delve deeper into the role of microglia in Alzheimer’s disease, neuroscientists Katherine Prater and Kevin Green of the University of Washington, along with colleagues from multiple US institutions, used brain autopsy samples from research donors — 12 with Alzheimer’s disease and 10 healthy people — to study the gene’s microglia activity. Small.
Using a new method of promotion Single-stranded RNA sequencingThe team was able to deeply identify 10 different populations of microglia in brain tissue based on their unique set of gene expression, which tells the cells what to do.
TThree groups had never been seen before, and one of them was more common in people with Alzheimer’s disease. This type of microglia contains genes that promote inflammation and cell death.
Overall, the researchers found that the populations of microglia in the brains of people with Alzheimer’s disease were more likely to be in a proinflammatory state.
This means they were more likely to produce inflammatory molecules that can damage brain cells and possibly contribute to the development of Alzheimer’s disease.
The types of microglia found in the brains of people with Alzheimer’s were less likely to be protective, affecting their ability to pull their weight cleaning up dead cells and waste and promoting healthy brain aging.
Scientists also believe that microglia can change types over time. So we can’t just look at a person’s brain and say for sure what type of microglia they have; Tracking how microglia change over time can help us understand how they contribute to Alzheimer’s disease.
“At this point, we cannot say whether it is the microglia that are causing the disease or whether it is the pathology that is causing the behavior of these microglia to change.” He said Prater.
This research is still in its early stages, but it advances our understanding of the role of these cells in Alzheimer’s disease and suggests that some populations of microglia may be targets for new treatments.
The team hopes that their work will lead to the development of new treatments that can improve the lives of people with Alzheimer’s disease.
“Now that we have identified the genetic profiles of these microglia, we can try to figure out exactly what they do, and hopefully identify ways to change their behaviors that may contribute to Alzheimer’s disease,” Prater says. He said.
“If we can determine what they are doing, we may be able to change their behavior with treatments that may prevent or slow this disease.”
The study was published in Aging nature.
A previous version of this article was published in August 2023.

“Amateur organizer. Wannabe beer evangelist. General web fan. Certified internet ninja. Avid reader.”



/cdn.vox-cdn.com/uploads/chorus_asset/file/25550621/voultar_snes2.jpg)


More Stories
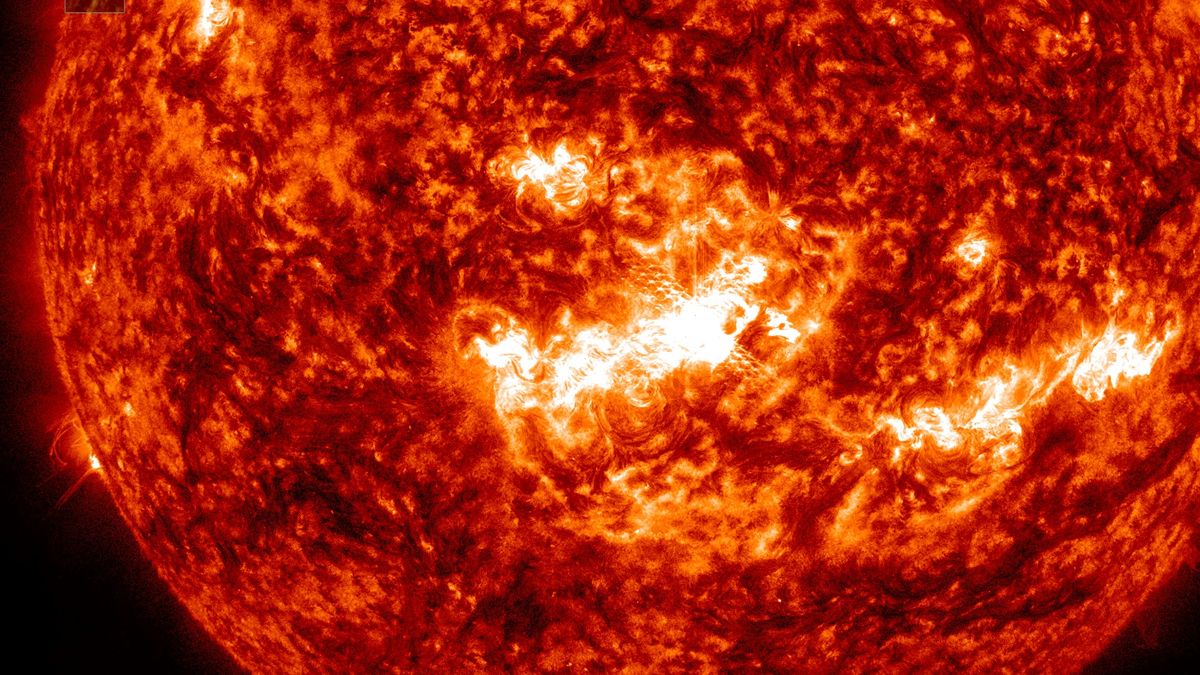
Watch a Massive X-Class Solar Explosion From a Sunspot Facing Earth (Video)
New Study Challenges Mantle Oxidation Theory
The theory says that complex life on Earth may be much older than previously thought.